Livanta
Livanta is responsible for the quality of care review of services provided to Massachusetts Medicare patients enrolled in Medicare Advantage products with CMS. This includes Tufts Medicare Preferred HMO members.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) of 1985, as amended by the Omnibus Budget Reconciliation Act (OBRA) of 1986, requires Tufts Health Plan to participate in an external review of its QI program for members enrolled in Tufts Medicare Preferred HMO. The responsibilities of each organization that conducts the external review of the Tufts Medicare Preferred HMO plan are delineated in the Tufts Health Plan/Livanta agreement.
The Livanta Bene ciary and Family Centered Care Quality Improvement Organization (BFCC-QIO) handles all Medicare bene ciary complaints, quality of care reviews, medical necessity reviews, and discharge appeals from hospitals, skilled nursing facilities, home health and hospice providers, and rehabilitation facilities. Medicare patients have certain rights and protections, and Livanta is here to help.
Livanta is the new Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) for Medicare case review. Livanta handles all appeals and quality of care complaints for people on Medicare who live in Massachusetts.
Livanta is Your QIO for Case Review
WHAT IS LIVANTA?
Livanta is a company that helps its customers by providing services like consulting in health care, program integrity, health technology and information, quality improvement, business process and outsourcing and strategic solutions for communications in the public sector and for health care consumers. The company helps store, protect and analyze large volumes of sensitive records of health care data of the American people to help the healthcare system function with proper integrity.
APPEAL FOR CLAIM
Livanta appeal can be made if a beneficiary thinks that his or her Medicare services are coming to an end too soon. For example, if the patient is told that his or her nursing home is discharging him or her, but the patient does not feel healthy enough for leaving. If the individual wishes to file an appeal regarding the situation, one can contact on the Livanta appeal phone number. The appeal usually relates to any request for review and one can contact the Livanta appeal address, process, phone number and they will provide quality and beneficent medical cover for the case reviews and also appropriate if the health services provided to the individual are according to the professional recognized care standards defined.
Appeals
• An appeal can be led if you think your Medicare services are ending too soon.
For example, you are told the nursing home is discharging you, but you do not feel healthy enough to leave.
• If you wish to le an appeal, call Livanta at 1-866-815-5440.
** An appeal relates to a request for review (for example, you are told the nursing home is discharging you and will no longer cover your stay, but you do not feel healthy enough to leave)
** If you wish to file an appeal, call Livanta at 866-815-5440 and select Option 1
Complaints
• A complaint relates to a concern about the quality of care or other services you get from a Medicare provider. For example, you developed a hospital-acquired infection and did not receive treatment.
• If you wish to le a complaint, call Livanta at 1-866-815-5440.
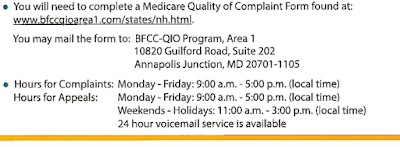
• You will need to complete a Medicare Quality of Complaint Form found at:
www.bfccqioarea1.com/states/ct.html.
You may mail the form to: BFCC-QIO Program, Area 1
9090 Junction Dr., Suite 10
Annapolis Junction, MD 20701
• Hours for Complaints: Monday - Friday: 9:00 a.m. - 5:00 p.m. (local time)
Hours for Appeals: Monday - Friday: 9:00 a.m. - 5:00 p.m. (local time)
Weekends - Holidays: 11:00 a.m. - 3:00 p.m. (local time)
24 hour voicemail service is available
Livanta appeal address
Helpful Tips
Have the following information
handy when you call:
** Medicare card
** Medicare number
** Address and phone number
** Date of birth
** Date of service
** Full name and contact information of the facility or healthcare provider
Billing
Livanta is not responsible for Medicare billing. If you have questions regarding your bill, please call 1-800-MEDICARE
FILING OF COMPLAINTS
A complaint is filed that relates to concerns about the quality and hospitality of care and any other service received from the Medicare provider. A good example would be developing an infection or disease in hospital and not receiving treatment for it. To file a complaint one can approach Livanta and rest assured all your services will be taken care of. One can also check their Livanta appeal status and can also file Livanta second appeal if the individual feels his or her service was not properly addressed during the first appeal.
To file a complaint, one must complete the Medicare Quality of Complaint Form that can be found on their website and this must be mailed to the concerned company for further checking of the claim or appeal. Most companies have specific hours for filing of appeals or complaints, but provide a 24 hour round the clock, voicemail service for the benefit of the people.
TIPS TO BE TAKEN CARE OF
The individual must possess the mentioned information at hand when he or she calls to file an appeal or complaint like the Medicare card, Medicare number, personal address and phone number, date of birth, date of the service, full name along with contact information of the concerned health care provider or facility. Livanta will not be responsible for the Medicare billing and for queries regarding the billing one can call the helpline number mentioned online.
Livanta also maintains a good review system that ensures that the services provided to the Medicare beneficiaries who are enrolled in various health plans in Medicare are of sufficient quality across all the settings. The review system of Livanta addresses issues like appropriateness of the treatment, accessibility to various services, timeliness of the provided services, potential for the under-utilization of the services, potential for the premature discharge of the patient etc.
LIVANTA APPEAL STATUS
One can check their Livanta appeal status by calling the Livanta appeal phone number which is the Livanta Medicare helpline
1877-588-1123. To check the status of Short Stay Reviews one must call at
1866-603-0970. The Livanta second appeal
can also be checked by calling on the mentioned helpline numbers.
Livanta Reviews
Livanta maintains a review system to ensure that services provided to Medicare beneficiaries enrolled in Medicare health plans are of adequate quality across all settings. This review system addresses the following issues:
** Appropriateness of treatment
** Potential for under-utilization of services
** Accessibility to services
** Potential for premature discharge of patients
** Timeliness of services provided
** Appropriateness of the setting for the provision of services
** Appropriateness of the Medicare health plan’s activities to coordinate care, such as the adequacy of discharge planning and follow-up of abnormal diagnostic studies
Livanta will notify Tufts Health Plan Medicare Preferred regarding issues that include results of Livanta’s review activities, unless otherwise specified in the Livanta/CMS contract. These issues will be identified as Quality of Care concerns or documentation concerns.
Tufts Health Plan Medicare Preferred will be notified when a Livanta review indicates a quality problem regarding an out-of-plan emergency or urgently needed care that an out-of-plan hospital, skilled nursing facility (SNF), or other health care facility provided to a Tufts Medicare Preferred HMO member, and the problem is attributable to the institution. However, the quality problem identified with respect to these services will be attributed to the out-of-plan provider/practitioner, rather than to Tufts Health Plan Medicare Preferred.
Quality Improvement Organization Complaint Process
For Tufts Medicare Preferred HMO members concerned about the quality of the care received can also file a complaint with Livanta at 866.815.5440. Quality Improvement Organizations (QIO), such as Livanta, are groups of doctors and health professionals that monitor the quality of care provided to Medicare beneficiaries. Livanta Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) for Massachusetts. The Livanta review process is designed to help prevent any improper practices. This process is separate and distinct from the Tufts Medicare Preferred HMO grievance (complaint) process.
The QIO is under contract to the CMS to conduct medical reviews and other functions with respect to Medicare beneficiaries.



No comments:
Post a Comment